Melatonin and Covid-19: An opened Pandora's box and the hope for the time being
Melatonin and COVID-19
Abstract
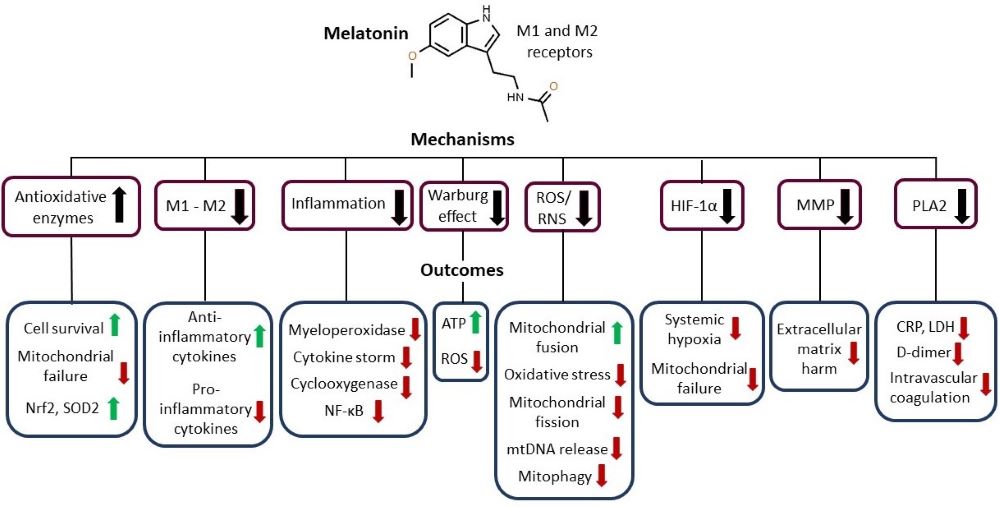
The SARS-CoV-2 pandemic is a global health concern still ongoing. No single therapeutic intervention with high efficacy exists and virus mutations continue to improve immune evasion decreasing vaccine efficacy. Therefore, a therapy which instead targets severe symptoms of COVID-19 should be contemplated. Hyperinflammation, cytokine storm and oxidation are relevant in the evolution of COVID-19. Considering the anti-inflammatory, anti-oxidative and cytoprotective effects of melatonin (MEL) on viral infections, its potential links with COVID-19 should be researched. In addition, evidence suggests a viricidal action of MEL and an increase in the efficacy of SARS-CoV-2 vaccines. One of the neglected and excellent options for therapy is MEL. We strongly support and encourage the use of MEL as a therapy for COVID-19.
References
2. Mohapatra RK, Verma S, Kandi V, Sarangi AK, Seidel C, Das SN, Behera A, Tuli HS, Sharma AK, Dhama K (2023) The SARS-CoV-2 Omicron variant and its multiple sub-lineages: Transmissibility, vaccine development, antiviral drugs, monoclonal antibodies, and strategies for infection control–A review. Chemistry Select. 8: e202201380. doi: 10.1002/slct.202201380.
3. Zhang R, Wang X, Ni L, Di X, Ma B, Niu S, Liu C, Reiter R.J (2020) COVID-19: Melatonin as a potential adjuvant treatment. Life Sci. 250: 117583. doi: 10.1016/j.1fs. 2020.117583.
4. Reiter RJ, Sharma R, Simko F, Dominguez-Rodriguez A, Tesarik J, Neel RL, Slominski AT, Kleszczynski K, Martin-Gimenez VM, Manucha W, Cardinali DP (2022) Melatonin: Highlighting its use as a potential treatment for SARS-CoV-2 infection. Cell. Mol. Life Sci. 79 (3): 143. doi: 10.1007/s00018-021-04102-3.
5. Kleszczyński K, Slominski AT, Steinbrink K, Reiter RJ (2020) Clinical trials for use of melatonin to fight against COVID-19 are urgently needed. Nutrients 12 (9): 2561. doi: 10.3390/nu12092561.
6. Vielma JR, Bonilla E, Chacín-Bonilla L, Mora M, Medina-Leendertz S, Bravo Y (2014) Effects of melatonin on oxidative stress, and resistance to bacterial, parasitic, and viral infections: A review. Acta Trop. 137: 31-38. doi: 10.1016/j.actatropica.2014.04.021.
7. Chacín-Bonilla L, Vielma JR, Bonilla E (2014) Should melatonin be considered a complementary or alternative therapy against parasitic infections?. Epidemiol. 4: e117. doi: 10.4172/2161-1165.1000e117.
8. Juybari KB, Pourhanifeh MH, Hosseinzadeh A, Hemati K, Mehrzadi S (2020) Melatonin potentials against viral infections including COVID-19: Current evidence and new findings. Virus Res. 287: 198108. doi: 10.1016%2Fj.virusres.2020.198108.
9. Cárdenas R, Chacín-Bonilla L, Bonilla E (2023) Melatonin: A review of its physiopathological and therapeutic relationship with parasitic diseases. Melatonin Res. 6 (1) 28-50. doi: 10.32794/mr112500139.
10. Reiter RJ, Ma Q, Sharma R (2020) Treatment of Ebola and other infectious diseases: Melatonin “goes viral”. Melatonin Res. 3 (1): 43-57. doi: 10.32794/mr11250047.
11. Kitidee K, Samutpong A, Pakpian N, Wisitponchai T, Govitrapong P, Reiter RJ, Wongchitra P (2023) Antiviral effect of melatonin on Japanese encephalitis virus infection involves inhibition of neuronal apoptosis and neuroinflammation in SH-SY5Y cells. Sci. Rep. 13: 6063. doi: 10.1038/s41598-023-33254-4.
12. Cardinali DP, Brown GM, Pandi-Perumal SR (2020) Can melatonin be a potential "silver bullet" in treating COVID-19 patients? Diseases 26: 8 (4): 44. doi: 10.3390/ diseases8040044.
13. Vlachou M, Siamidi A, Dedeloudi A, Konstantinidou SK, Papanastasiou IP (2021) Pineal hormone melatonin as an adjuvant treatment for COVID 19. Int. J. Mol. Med. 47 (4): 47. doi: 10.3892/ijmm.2021.4880.
14. Bonilla E, Valero N, Ponds H, Chacín-Bonilla L (1997) Melatonin protects mice infected with Venezuelan equine encephalomyelitis virus. Cell Mol. Life Sci. 53 (5): 430-434. doi: 10.1007/s000180050051.
15. Medina S, Valero-Fuenmayor N, Chacín-Bonilla L, Anez F, Giraldoth D, Arias J, Espina G, Achong AY, Bonilla E (1999) Exposure to 2500 lux increases serum melatonin in Venezuelan equine encephalomyelitis. Neurochem. Res. 24 (6): 775-778. doi: 10.1023/a:1020735730869.
16. Bonilla E, Rodón C, Valero N, Pons H, Chacín-Bonilla L, Tamayo JG, Rodríguez Z, Medina-Leendertz S, Añez F (2001) Melatonin prolongs survival of immunodepressed mice infected with the Venezuelan equine encephalomyelitis virus. Trans. R. Soc. Trop. Med. Hyg. 95 (2): 207-210. doi: 10.1016/s0035-9203(01)90170-1.
17. Arias J, Meleán E, Valero N, Ponds H, Chacín-Bonilla L, Larreal Y, Bonilla E (2003) Efecto de la melatonina en la proliferación linfocitaria y la producción de interleucina 2 (IL-2) e interleucina 1 beta (IL-1β) en esplenocitos de ratones. Invest. Clin. 44 (1): 41-50.
18. Bonilla E, Valero N, Chacín-Bonilla L, Pons H, Larreal Y, Medina-Leendertz S, Marina Espina L (2003) Melatonin increases interleukin-1β and decreases tumor necrosis factor alpha in the brain of mice infected with the Venezuelan equine encephalomyelitis virus. Neurochem. Res. 28 (5): 681-686. doi: 10.1023/a:1022897314108.
19. Valero N, Meleán E, Bonilla E, Arias J, Espina LM, Chacín-Bonilla L, Larreal Y, Maldonado M, Anez F (2005) In vitro, melatonin treatment decreases nitric oxide levels in murine splenocytes cultured with the Venezuelan equine encephalomyelitis virus. Neurochem. Res. 30 (11): 1439-1442. doi: 10.1007/s11064-005-8634-1.
20. Montiel M, Bonilla E, Valero N, Mosquera J, Espina LM, Quiroz Y, Álvarez‐Mon M (2015) Melatonin decreases brain apoptosis, oxidative stress, and cd200 expression and increased survival rate in mice infected by Venezuelan equine encephalitis virus. Antivir. Chem. Chemother. 24 (3-4): 99‐108. doi: 10.1177/2040206616660851.
21. Bonilla E, Valero N, Chacín-Bonilla L, Medina-Leendertz S (2004) Melatonin and viral infections. J. Pineal Res. 36 (2): 73-79. doi: 10.1046/j.1600-079x.2003.00105.x.
22. Tan DX, Hardeland R (2020) Potential utility of melatonin in deadly infectious diseases related to the overreaction of innate immune response and destructive inflammation: Focus on COVID-19. Melatonin Res. 3 (1): 120-143. doi:10.32794/ mr11250052.
23. Codo AC, et al. (2020) Elevated glucose levels favor SARS-CoV-2 infection and monocyte response through a HIF-1α/glycolysis-dependent axis. Cell Metab. 32 (3): 437-446.e5. doi: 10.1016/j.cmet.2020.07.007.
24. Hardeland R (2018) Melatonin and inflammation-story of a double-edged blade. J. Pineal Res. 65 (4): e12525. doi: 10.1111/jpi.12525.
25. Cheng J, Yang HL, Gu CJ, Liu YK, Shao J, Zhu R, He YY, Zhu XY, Li MQ (2019) Melatonin restricts the viability and angiogenesis of vascular endothelial cells by suppressing HIF-1α/ROS/VEGF. Int. J. Mol. Med. 43 (2): 945-955. doi:10.3892/ijmm. 2018.4021.
26. Kücükakin B, Lykkesfeldt J, Nielsen HJ, Reiter RJ, Rosenberg J, Gögenur I (2008) Utility of melatonin to treat surgical stress after major vascular surgery-a safety study. J. Pineal Res. 44 (4): 426-431. doi: 10.1111/j.1600-079X.2007.00545.x.
27. Zhao Z, Lu C, Li T, Wang W, Ye W, Zeng R, Ni L, Lai Z, Wang X, Liu C (2018). The protective effect of melatonin on brain ischemia and reperfusion in rats and humans: In vivo assessment and a randomized controlled trial. J. Pineal Res. 65 (4): e12521. doi: 10.1111/jpi.12521.
28. Bazyar H, Gholinezhad H, Moradi L, Salehi P, Abadi F, Ravanbakhsh M, Zare Javid A (2019) The effects of melatonin supplementation in adjunct with non-surgical periodontal therapy on periodontal status, serum melatonin and inflammatory markers in type 2 diabetes mellitus patients with chronic periodontitis: A double-blind, placebo-controlled trial. Inflammopharmacology 27 (1): 67-76. doi: 10.1007/s10787-018-0539-0.
29. Sánchez-López AL, Ortiz GG, Pacheco-Moises FP, Mireles-Ramírez MA, Bitzer-Quintero OK, Delgado-Lara DLC, Ramírez-Jirano LJ, Velázquez-Brizuela IE (2018) Efficacy of melatonin on serum pro-inflammatory cytokines and oxidative stress markers in relapsing remitting multiple sclerosis. Arch. Med. Res. 49 (6): 391-398. doi:10.1016/ j.arcmed.2018.12.004.
30. Maroufi NF, Amiri M, Dizaji BF, Vahedian V, Akbarzadeh M, Roshanravan N, Haiaty S, Nouri M, Rashidi MR (2020) Inhibitory effect of melatonin on hypoxia-induced vasculogenic mimicry via suppressing epithelial-mesenchymal transition (EMT) in breast cancer stem cells. Eur. J. Pharmacol. 881: 173282. doi: 10.1016/j.ejphar.2020.173282.
31. Zonta YR, Martinez M, Camargo IC, Domeniconi RF, Lupi Junior LA, Pinheiro PF, Reiter RJ, Martinez FE, Chuffa LG (2017) Melatonin reduces angiogenesis in serous papillary ovarian carcinoma of ethanol-preferring rats. Int. J. Mol. Sci. 11 (4): 763. doi: 10.3390/ijms18040763.
32. Ling Y, Li ZZ, Zhang JF, Zheng XW, Lei ZQ, Chen RY, Feng JH (2018) MicroRNA-494 inhibition alleviates acute lung injury through Nrf2 signaling pathway via NQO1 in sepsis-associated acute respiratory distress syndrome. Life Sci. 210: 1-8. doi:10.1016/ j.lfs.2018.08.037.
33. Ahmadi Z, Ashrafizadeh M (2020) Melatonin as a potential modulator of Nrf2. Fundam. Clin. Pharmacol. 34 (1): 11-19. doi: 10.1111/fcp.12498.
34. Reiter RJ, Sharma R, Rosales-Corral S (2021) Anti-Warburg effect of melatonin: a proposed mechanism to explain its inhibition of multiple diseases. Int. J. Mol. Sci. 22 (2): 764. doi:10.3390/ijms22020764.
35. Begum R, Mamun-Or-Rashid ANM, Lucy TT, Pramanik MK, Sil BK, Mukerjee N, Tagde P, Yagi M, Yonei Y (2022) Potential therapeutic approach of melatonin against Omicron and some other variants of SARS-CoV-2. Molecules 27 (20): 6934. doi: 10.3390/molecules27206934.
36. Chitimus DM, Popescu MR, Voiculescu SE, Panaitescu AM, Pavel B, Zagrean L, Zagrean AM (2020) Melatonin's impact on antioxidative and anti-Inflammatory reprogramming in homeostasis and disease. Biomolecules 10 (9): 1211. doi:10.3390/ biom10091211.
37. Yim J, Lim HH, Kwon Y (2021) COVID-19 and pulmonary fibrosis: Therapeutics in clinical trials, repurposing, and potential development. Arch. Pharm. Res. 44 (5): 499-513. doi: 10.1007/s12272-021-01331-9.
38. Souissi A, Dergaa I, Romdhani M, Ghram A, Irandoust K, Chamari K, Ben Saad H (2023) Can melatonin reduce the severity of post-COVID-19 syndrome? EXCLI J. 22:173-187. doi: 10.17179/excli2023-5864.
39. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B (2020) Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 77 (6): 683-690. doi:10.1001/jamaneurol. 2020.1127.
40. Sundberg I, Ramklint M, Stridsberg M, Papadopoulos FC, Ekselius L, Cunningham JL (2016) Salivary melatonin in relation to depressive symptom severity in young adults. PLoS One 11 (4): e0152814. doi: 10.1371/journal.pone.0152814.
41. Romero A, Ramos E, López-Muñoz F, Gil-Martín E, Escames G, Reiter RJ (2022) Coronavirus disease 2019 (COVID-19) and its neuroinvasive capacity: Is it time for melatonin? Cell Mol. Neurobiol. 42 (3): 489-500. doi: 10.1007/s10571-020-00938-8.
42. Valero N, Nery A, Bonilla E, Espina LM, Chacín-Bonilla L, Anez F, Maldonado M, Meleán E (2009) Antagonistic effect of luzindole in mice treated with melatonin during the infection with the Venezuelan equine encephalomyelitis virus. Neurochem. Res. 34 (2): 268-273. doi: 10.1007/s11064-008-9766-x.
43. Ramos E, López-Muñoz F, Gil-Martín E, Egea J, Álvarez-Merz I, Painuli S, Semwal P, Martins N, Hernández-Guijo JM, Romero A (2021) The coronavirus disease 2019 (COVID-19): Key emphasis on melatonin safety and therapeutic efficacy. Antioxidants 10 (7): 1152. doi: 10.3390/antiox10071152.
44. Chacín-Bonilla L, Cardenas R, Bonilla E (2022) Melatonin: The continuing neuroprotective promise of a versatile molecule. Int. J. Case Rep. 8 (1): 9-12. doi: 10.37871/ijcrsr.id99.
45. Molina-Carballo A, Palacios-López R, Jerez-Calero A, Augustín-Morales MC, Agil A, Muñoz-Hoyos A, Muñoz-Gallego A (2021) Protective effect of melatonin administration against SARS-CoV-2 infection: A systematic review. Curr. Issues Mol. Biol. 44 (1): 31-45. doi: 10.3390/cimb44010003.
46. Negrette B, Bonilla E, Valero N, Pons H, Tamayo JG, Chacín-Bonilla L, Medina- Leendertz S, Añez F (2001) Melatonin treatment enhances the efficiency of mice immunization with Venezuelan equine encephalomyelitis virus TC-83. Neurochem. Res. 26 (7): 767-770. doi: 10.1023/a:1011645400123.
47. Chacín-Bonilla L, Dikdan Y (1981) Prevalencia de Entamoeba histolytica y otros parásitos intestinales en una comunidad suburbana de Maracaibo. Invest. Clín. 22 (4): 185-203.
48. Chacín-Bonilla L, Mathews H, Dikdan Y, Guanipa N (1990) Estudio seroepidemiológico de la amibiasis en una comunidad del estado Zulia, Venezuela. Rev. Inst. Med. Trop. Sao Paulo 32 (6): 467-473.
49. Chacín-Bonilla L, Sánchez Y, Estévez J, Larreal Y, Molero E (2003) Prevalence of human toxoplasmosis in San Carlos Island, Venezuela. Interciencia 28 (8): 457-462.
50. Abdoli A (2020) Helminths and COVID-19 co-infections: A neglected critical challenge. ACS Pharmacol. Transl. Sci. 3 (5): 1039-1041. doi: 10.1021/acsptsci.0c00141.
51. Chacon N, Chacín-Bonilla L, Cesari IM (2021) Implications of helminth immunomodulation on COVID-19 co-infections. Life Res. 4 (3): 26. doi: 10.53388/life 2021-0502-309.
52. Chacín-Bonilla L, Chacon-Fonseca N, Rodriguez-Morales A (2021) Emerging issues in COVID-19 vaccination in tropical areas: Impact of the immune response against helminths in endemic areas. Travel Med. Infect. Dis. 42: 102087. doi:10.1016/j.t maid.2021.102087.
53. Martín Giménez VM, Modrego J, Gómez-Garre D, Manucha W, de Las Heras N (2023) Gut microbiota dysbiosis in COVID-19: Modulation and approaches for prevention and therapy. Int, J, Mol, Sci. 24 (15):12249. doi: 10.3390/ijms241512249.
54. Anderson G, Reiter RJ (2020) Melatonin: Roles in influenza, Covid-19, and other viral infections. Rev. Med. Virol. 30 (3): e2109. doi: 10.1002/rmv.2109.
55. Panda SR, Chaudhari VB, Ahmed S, Kwatra M, Jala A, Ponneganti S, Pawar SD, Borkar RM, Sharma P, Naidu VGM (2023) Ambient particulate matter (PM2.5) exposure contributes to neurodegeneration through the microbiome-gut-brain axis: Therapeutic role of melatonin. Environ. Toxicol. Pharmacol. 101:104183. doi: 10.1016/j.etap.2023.104183.
56. Wang X, Wang Z, Cao J, Dong Y, Chen Y (2023) Gut microbiota-derived metabolites mediate the neuroprotective effect of melatonin in cognitive impairment induced by sleep deprivation. Microbiome 2023 11 (1):17. doi: 10.1186/s40168-022-01452-3.
57. Nicese MN, Bijkerk R, Van Zonneveld AJ, Van den Berg BM, Rotmans JI (2023) Sodium butyrate as key regulator of mitochondrial function and barrier integrity of human glomerular endothelial cells. Int. J. Mol. Sci. 24 (17):13090. doi: 10.3390/ijms241713090.
58. Jin CJ, Engstler AJ, Sellmann C, Ziegenhardt D, Landmann M, Kanuri G, Lounis H, Schröder M, Vetter W, Bergheim I (2016) Sodium butyrate protects mice from the development of the early signs of non-alcoholic fatty liver disease: role of melatonin and lipid peroxidation. Br. J. Nutr. 23:1-12. doi: 10.1017/S000711451600402559.
59. Anderson G, Almulla AF, Reiter RJ, Maes M (2023) Redefining autoimmune disorders' pathoetiology: Implications for mood and psychotic disorders' association with neurodegenerative and classical autoimmune disorders. Cells 12 (9): 1237. doi: 10.3390/cells12091237.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


