Melatonin as a microenvironmental cue for parasite development inside the host
Melatonin interactions in the host-parasite relationship
Abstract
Throughout the evolutionary process, parasites have
acquired characteristics that function as survival mechanisms. It has been
reported that melatonin, a molecule present in virtually all living organisms,
has several roles in parasite biology such as preventing tissue damage,
regulating gene expression and inflammatory processes, and acting as a free
radical scavenger. Additionally,
melatonin produced by the hosts accelerates the intra-erythrocytic cycle of the
human malaria parasite Plasmodium falciparum and the rodent malaria
parasite P. chabaudi, respectively. These findings have recently led to
an increased research enthusiasm to find how melatonin influences the
biological cycle of parasites. Therefore, this review aims to gather and
analyze the potential relationships of host produced melatonin with the
parasites Plasmodium sp., Trypanosoma cruzi, Leishmania
spp., Toxoplasma gondii, Schistosoma mansoni, Opisthorchis viverrini, and Entamoeba
histolytica, respectively.
References
2. Galano A, Tan DX, Reiter RJ (2011) Melatonin as a natural ally against oxidative stress: a physicochemical examination. J. Pineal Res. 1: 1-16. DOI: 10.1111/j.1600-079X.2011.00916.x. PMID: 21752095.
3. Hardeland R, Poeggeler B (2008) Melatonin Beyond Its Classical Functions. Open Physiol. J. 1: 1-22. DOI: 10.2174/1874360900901010001.
4. Leite AA, Reiter RJ, Brandão JCM, Sakae TM, Marinho M, Camargo CR, Oliveira-Junior IS (2021) Melatonin can be, more effective than N-acetylcysteine, protecting acute lung injury induced by intestinal ischemia-reperfusion in rat model. Clinics 76: e2513 DOI: 10.6061/CLINICS/2021/E2513.
5. Ren BC, Zhang W, Zhang W, Ma JX, Pei F, Li BY (2021) Melatonin attenuates aortic oxidative stress injury and apoptosis in STZ-diabetes rats by Notch1/Hes1 pathway. J. Steroid Biochem. Mo.l Biol. 212: 105948. DOI: 10.1016/J.JSBMB.2021.105948.
6. Sadoughi F, Dana PM, Asemi Z, Shafabakhash R, Mohammadi S, Heidar Z, Mirzamoradi M, Targhazeh N, Mirzaei H (2022) Molecular and cellular mechanisms of melatonin in breast cancer. Biochimie S0300-9084(22)00067-0. DOI: 10.1016/j.biochi.2022.03.005.
7. Guerra J, Devesa J. (2022) Usefulness of Melatonin and Other Compounds as Antioxidants and Epidrugs in the Treatment of Head and Neck Cancer. Antioxidants 11 (1): 35. DOI: 10.3390/antiox11010035.
8. Ashrafizadeh M, Ahmadi Z, Yaribeygi H, Sathyapalan T, Jamialahmadi T, Sahebkar A (2021) Antitumor and Protective Effects of Melatonin: The Potential Roles of MicroRNAs. Adv. Exp. Med. Bio. 1328: 463-471. DOI: 10.1007/978-3-030-73234-9_3.1
9. Lim S, Park S, Koyanagi A, Yang JW, Jacob L, Yon DK, Lee SW, Kim MS, Il Shin J, Smith L (2022) Effects of exogenous melatonin supplementation on health outcomes: An umbrella review of meta-analyses based on randomized controlled trials. Pharmacol. Res. 176: 106052. DOI: 10.1016/j.phrs.2021.106052.
10. Reiter RJ, Sharma R, Simko F, Dominguez-Rodriguez A, Tesarik J, Neel RL, Slominski AT, Kleszczynski K, Martin-Gimenez VM, Manucha W, Cardinali DP (2022) Melatonin: highlighting its use as a potential treatment for SARS-CoV-2 infection. Cell. Mol. Life Sci. 3: 143. DOI: 10.1007/s00018-021-04102-3.
11. Tan DX, Reiter RJ (2022) Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality. Life Sci. 294: 120368. DOI: 10.1016/j.lfs.2022.120368.
12. Li L, Gang X, Wang J, Gong X (2022) Role of melatonin in respiratory diseases. Exp. Ther. Med. 4: 271. DOI: 10.3892/etm.2022.11197.
13. Reppert SM, Weaver DR, Ebisawa T (1994) Cloning and characterization of a mammalian melatonin receptor that mediates reproductive and circadian responses. Neuron 13: 1177–1185. DOI: 10.1016/0896-6273(94)90055-8.
14. Reppert SM, Godson C, Mahle CD, Weaver DR, Slaugenhaupt SA, Gusella JF (1995) Molecular characterization of a second melatonin receptor expressed in human retina and brain: the Mel1b melatonin receptor. Proc. Natl. Acad. Sci. USA 92: 8734–8738. DOI: 10.1073/PNAS.92.19.8734.
15. Petit L, Lacroix I, de Coppet P, Strosberg AD, Jockers R (1999) Differential signaling of human Mel1a and Mel1b melatonin receptors through the cyclic guanosine 3’-5’-monophosphate pathway. Biochem. Pharmacol. 58: 633–639. DOI: 10.1016/S0006-2952(99)00134-3.
16. Lerner AB, Case JD, Takahashi Y, Lee TH, Mori W (1958) Isolation of melatonin, the pineal gland factor that lightens melanocytes. J. Am. Chem. Soc. 80: 2587. DOI: 10.1021/JA01543A060.
17. Reiter RJ, Tan DX, Kim SJ, Cruz MH (2014) Delivery of pineal melatonin to the brain and SCN: role of canaliculi, cerebrospinal fluid, tanycytes and Virchow-Robin perivascular spaces. Brain Struct.Funct. 6: 1873-87. DOI: 10.1007/s00429-014-0719-7.
18. Tan DX, Manchester LC, Reiter RJ (2016) CSF generation by pineal gland results in a robust melatonin circadian rhythm in the third ventricle as an unique light/dark signal. Med. Hypotheses. 86: 3-9. DOI: 10.1016/j.mehy.2015.11.018.
19. Bitar RD, Torres-Garza JL, Reiter RJ, Phillips WT (2021) Neural glymphatic system: Clinical implications and potential importance of melatonin. Mel. Res. 4: 551-565. DOI:https://doi.org/https://doi.org/10.32794/mr112500111.
20. Stefulj J, Hörtner M, Ghosh M, Schauenstein K, Rinner I, Wölfler A, Semmler J, Liebmann PM (2001) Gene expression of the key enzymes of melatonin synthesis in extrapineal tissues of the rat. J. Pineal Res. 4: 243-7. DOI: 10.1034/j.1600-079x.2001.300408.x.
21. Sanchez-Hidalgo M, de la Lastra CA, Carrascosa-Salmoral MP, Naranjo MC, Gomez-Corvera A, Caballero B, Guerrero JM (2009) Age-related changes in melatonin synthesis in rat extrapineal tissues. Exp. Gerontol. 5: 328-34. DOI: 10.1016/j.exger.2009.02.002.
22. Bubenik GA (2002) Gastrointestinal melatonin: localization, function, and clinical relevance. Dig. Dis. Sci. 10: 2336-48. DOI: 10.1023/a:1020107915919. PMID: 12395907.
23. Acuña-Castroviejo D, Escames G, Venegas C, Díaz-Casado ME, Lima-Cabello E, López LC, Rosales-Corral S, Tan DX, Reiter RJ (2014) Extrapineal melatonin: sources, regulation, and potential functions. Cell. Mol. Life Sci. 16: 2997-3025. DOI: 10.1007/s00018-014-1579-2.
24. Tan DX, Manchester LC, Liu X, Rosales-Corral SA, Acuna-Castroviejo D, Reiter RJ (2013) Mitochondria and chloroplasts as the original sites of melatonin synthesis: a hypothesis related to melatonin's primary function and evolution in eukaryotes. J. Pineal Res. 2: 127-38. DOI: 10.1111/jpi.12026.
25. Anderson G (2019) Gut Dysbiosis Dysregulates Central and Systemic Homeostasis via Decreased Melatonin and Suboptimal Mitochondria Functioning: Pathoetiological and Pathophysiological Implications. Mel. Res. 2: 70-85. DOI: 10.32794/mr11250022.
26. Anderson G (2020) Tumour Microenvironment: Roles of the Aryl Hydrocarbon Receptor, O-GlcNAcylation,Acetyl-CoA and Melatonergic Pathway in Regulating Dynamic Metabolic Interactions across Cell Types-Tumour Microenvironment and Metabolism. Int. J. Mol. Sci. 1: 141. DOI: 10.3390/ijms22010141. PMID: 33375613; PMCID: PMC7795031.
27. Klein DC (2007) Arylalkylamine N-acetyltransferase: “The timezyme.” J. Biol. Chem. 282: 4233–4237. DOI: 10.1074/jbc.R600036200.
28. Ganguly S, Coon SL, Klein DC (2002) Control of melatonin synthesis in the mammalian pineal gland: The critical role of serotonin acetylation. Cell Tissue Res. 309: 127–137. DOI: 10.1007/s00441-002-0579-y.
29. Ho AK, Thomas TP, Chik CL, Anderson WB, Klein DC (1988) Protein kinase C: Subcellular redistribution by increased Ca2+ influx. Evidence that Ca2+-dependent subcellular redistribution of protein kinase C is involved in potentiation of β-adrenergic stimulation of pineal cAMP and cGMP by K+ and A23187. J. Biol. Chem. 263: 9292–9297. DOI: 10.1016/s0021-9258(19)76538-7.
30. Sugden D, Vanecek J, Klein DC, Thomas TP, Anderson WB (1985) Activation of protein kinase C potentiates isoprenaline-induced cyclic AMP accumulation in rat pinealocytes. Nature 314: 359–361. DOI: 10.1038/314359a0.
31. Sugden LA, Sugden D, Klein DC (1987) Alpha 1-adrenoceptor activation elevates cytosolic calcium in rat pinealocytes by increasing net influx. J. Biol. Chem. 262: 741–745. DOI: 10.1016/S0021-9258(19)75847-5.
32. Ho AK, Klein DC (1987) Activation of alpha 1-adrenoceptors, protein kinase C, or treatment with intracellular free Ca2+ elevating agents increases pineal phospholipase A2 activity. Evidence that protein kinase C may participate in Ca2+-dependent alpha 1-adrenergic stimulation of pineal phospholipase A2 activity. J. Biol. Chem. 262: 11764–11770. DOI: 10.1016/S0021-9258(18)60877-4.
33. Sugden AL, Sugden D, Klein DC (1986) Essential role of calcium influx in the adrenergic regulation of cAMP and cGMP in rat pinealocytes. J. Biol. Chem. 261: 11608–11612. DOI: 10.1016/s0021-9258(18)67286-2.
34. Ganguly S, Gastel JA, Weller JL, Schwartz C, Jaffe H, Namboodiri MAA, Coon SL, Hickman AB, Rollag M, Obsil T, Beauverger P, Ferry G, Boutin JA, Klein DC (2001) Role of a pineal cAMP-operated arylalkylamine N-acetyltransferase14-3-3-binding switch in melatonin synthesis. Proc. Natl. Acad. Sci. USA 98: 8083-8088. DOI: 10.1073/PNAS.141118798.
35. Ganguly S, Weller JL, Ho A, Chemineau P, Malpaux B, Klein DC (2005) Melatonin synthesis: 14-3-3-dependent activation and inhibition of arylalkylamine N-acetyltransferase mediated by phosphoserine-205. Proc. Natl. Acad. Sci. USA 102: 1222-1227. DOI: 10.1073/PNAS.0406871102.
36. Pozdeyev N, Taylor C, Haque R, Chaurasia SS, Visser A, Thazyeen A, Du Y, Fu H, Weller J, Klein DC, Iuvone PM (2006) Photic regulation of arylalkylamine N-acetyltransferase binding to 14-3-3 proteins in retinal photoreceptor cells. J. Neurosci. 26: 9153–9161. DOI: 10.1523/JNEUROSCI.1384-06.2006.
37. World Health Organization (2020) World Malaria Report: 20 years of global progress and challenges. World Health Organization WHO/HTM/GM:299.
38. Sabbatani S, Fiorino S, Manfredi R (2010) The emerging of the fifth malaria parasite (Plasmodium knowlesi): a public health concern? Braz. J. Infect. Dis. 14: 299–309. DOI: 10.1590/s1413-86702010000300019.
39. Klein EY (2013) Antimalarial drug resistance: A review of the biology and strategies to delay emergence and spread. Int. J. Antimicrob. Agents 41: 311–317. DOI: 10.1016/j.ijantimicag.2012.12.007.
40. Mitchell GH, Bannister LH, Sinden RE (1988) Malaria parasite invasion: Interactions with the red cell membrane. Critic. Rev. Oncol. Hematol. 8: 255–310. DOI: 10.1016/S1040-8428(88)80011-8.
41. Cowman AF, Healer J, Marapana D, Marsh K (2016) Malaria: Biology and Disease. Cell 167: 610–624. DOI: 10.1016/J.CELL.2016.07.055.
42. Rijo-Ferreira F, Acosta-Rodriguez VA, Abel JH, Kornblum I, Bento I, Kilaru G, Klerman EB, Mota MM, Takahashi JS (2020) The malaria parasite has an intrinsic clock. Science 368: 746–753. DOI: 10.1126/science.aba2658.
43. Smith LM, Motta FC, Chopra G, Moch JK, Nerem RR, Cummins B, Roche KE, Kelliher CM, Leman AR, Harer J, Gedeon T, Waters NC, Haase SB (2020) An intrinsic oscillator drives the blood stage cycle of the malaria parasite Plasmodium falciparum. Science 368: 754–759. DOI: 10.1126/science.aba4357.
44. Trager W, Jensen JB (1976) Human malaria parasites in continuous culture. Science (New York, NY) 193: 673–675. DOI: 10.1126/SCIENCE.781840.
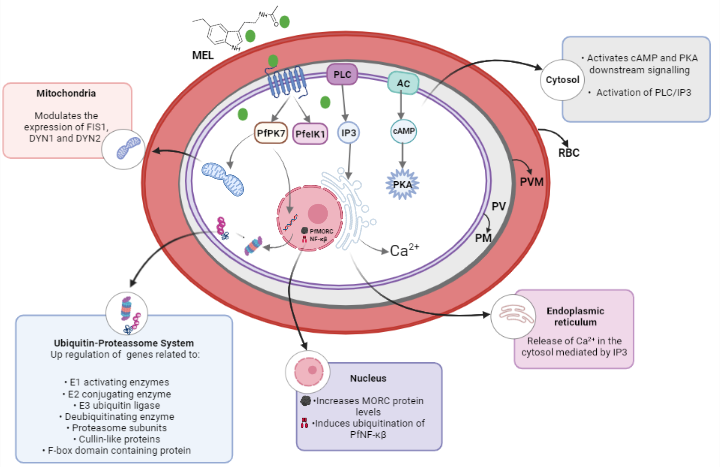
45. Hotta CT, Gazarini ML, Beraldo FH, Varotti FP, Lopes C, Markus RP, Pozzan T, Garcia CRS (2000) Calcium-dependent modulation by melatonin of the circadian rhythm in malarial parasites. Nat. Cell Biol. 2: 466-468. DOI: 10.1038/35017112.
46. Bagnaresi P, Alves E, da Silva HB, Epiphanio S, Mota MM, Garcia CRS (2009) Unlike the synchronous Plasmodium falciparum and P. chabaudi infection, the P. berghei and P. yoelii asynchronous infections are not affected by melatonin. Int. J. Gen. Med. 2: 47–55. DOI: 10.2147/ijgm.s3699.
47. Boyd GH (1929) Induced variations in the asexual cycle of Plasmodium cathemerium. Am. J. Epidemiol. 9: 81-187. DOI: 10.1093/oxfordjournals.aje.a121636.
48. David PH, Hommel M, Benichout J-C, Eisen HA, Silva LH (1978) Isolation of malaria merozoites: Release of Plasmodium chabaudi merozoites from schizonts bound to immobilized concanavalin A (rodent malaria/concanavalin A-Sepharose/merozoite isolation Proc. Natl. Acad. Sci. USA 75: 5081-5084. DOI: 10.1073/pnas.75.10.5081.
49. Alves E, Bartlett PJ, Garcia CRS, Thomas AP (2011) Melatonin and IP3-induced Ca2+ release from intracellular stores in the malaria parasite Plasmodium falciparum within infected red blood cells. J. Biol. Chem. 286: 5905–5912. DOI: 10.1074/jbc.M110.188474.
50. Beraldo FH, Garcia CRS (2005) Products of tryptophan catabolism induce Ca2+ release and modulate the cell cycle of Plasmodium falciparum malaria parasites. J. Pineal Res. 39: 224–230. DOI: 10.1111/j.1600-079X.2005.00249.x.
51. Schuck DC, Ribeiro RY, Nery AA, Ulrich H, Garcia CRS (2011) Flow cytometry as a tool for analyzing changes in Plasmodium falciparum cell cycle following treatment with indol compounds. Cytometry Part A 79 A: 959–964. DOI: 10.1002/cyto.a.21136.
52. Budu A, Peres R, Bueno VB, Catalani LH, Garcia CRS (2007) N1-acetyl-N2-formyl-5-methoxykynuramine modulates the cell cycle of malaria parasites. J. Pineal Res. 42: 261–266. DOI: 10.1111/j.1600-079X.2006.00414.x.
53. Schuck DC, Jordão AK, Nakabashi M, Cunha AC, Ferreira VF, Garcia CRS (2014) Synthetic indole and melatonin derivatives exhibit antimalarial activity on the cell cycle of the human malaria parasite Plasmodium falciparum. Eur. J. Med. Chem. 78: 375–382. DOI: 10.1016/J.EJMECH.2014.03.055
54. Dias BKM, Nakabashi M, Alves MRR, Portella DP, Santos BM, Almeida FCS, Ribeiro RY, Schuck DC, Jordão AK, Garcia CRS (2020) The Plasmodium falciparum eIK1 kinase (PfeIK1) is central for melatonin synchronization in the human malaria parasite. Melatotosil blocks melatonin action on parasite cell cycle. J. Pineal Res. 69: e12685. DOI: 10.1111/JPI.12685.
55. Beraldo FH, Almeida FM, da Silva AM, Garcia CR (2005) Cyclic AMP and calcium interplay as second messengers in melatonin-dependent regulation of Plasmodium falciparum cell cycle. J. Cell Biol. 170: 551–557. DOI: 10.1083/JCB.200505117.
56. Alves E, Bartlett PJ, Garcia CR, Thomas AP (2011) Melatonin and IP3-induced Ca2+ release from intracellular stores in the malaria parasite Plasmodium falciparum within infected red blood cells. J. Biol. Chem. 286: 5905–5912. DOI: 10.1074/JBC.M110.188474.
57. Furuyama W, Enomoto M, Mossaad E, Kawai S, Mikoshiba K, Kawazu SI (2014) An interplay between 2 signaling pathways: Melatonin-cAMP and IP 3-Ca2+ signaling pathways control intraerythrocytic development of the malaria parasite Plasmodium falciparum. Biochem. Biophys. Res. Commun. 446: 125–131. DOI: 10.1016/j.bbrc.2014.02.070.
58. Pecenin MF, Borges-Pereira L, Levano-Garcia J, Budu A, Alves E, Mikoshiba K, Thomas A, Garcia CRS (2018) Blocking IP3 signal transduction pathways inhibits melatonin-induced Ca2+ signals and impairs P. falciparum development and proliferation in erythrocytes. Cell Calcium 72: 81–90. DOI: 10.1016/j.ceca.2018.02.004.
59. Alves E, Nakaya H, Guimarães E, Garcia CRS (2021) Combining IP3 affinity chromatography and bioinformatics reveals a novel protein-IP3 binding site on Plasmodium falciparum MDR1 transporter. bioRxiv 2021.03.25.437059. DOI: 10.1101/2021.03.25.437059. Preprint, posted March 25, 2021.
60. Widmann C, Gibson S, Jarpe MB, Johnson GL (1999) Mitogen-activated protein kinase: Conservation of a three-kinase module from yeast to human. Physiol. Rev. 79: 143–180. DOI: 10.1152/PHYSREV.1999.79.1.143.
61. Garrington TP, Johnson GL (1999) Organization and regulation of mitogen-activated protein kinase signaling pathways. Curr. Opin. Cell Biol. 11: 211–218. DOI: 10.1016/S0955-0674(99)80028-3.
62. Raman M, Cobb MH (2003) MAP kinase modules: many roads home. Curr. Biol. 13: 886-888. DOI: 10.1016/J.CUB.2003.10.053.
63. Dorin D, Semblat JP, Poullet P, Alano P, Goldring JP, Whittle C, Patterson S, Chakrabarti D, Doerig C (2005) PfPK7, an atypical MEK-related protein kinase, reflects the absence of classical three-component MAPK pathways in the human malaria parasite Plasmodium falciparum. Mol. Microbiol. 55: 184–186. DOI: 10.1111/J.1365-2958.2004.04393.X.
64. Dorin-Semblat D, Sicard A, Doerig C, Ranford-Cartwright L, Doerig C (2008) Disruption of the PfPK7 gene impairs schizogony and sporogony in the human malaria parasite Plasmodium falciparum. Eukaryot. cell 7: 279–285. DOI: 10.1128/EC.00245-07.
65. Koyama FC, Ribeiro RY, Garcia JL, Azevedo MF, Chakrabarti D, Garcia CRS (2012) Ubiquitin Proteasome System and the atypical kinase PfPK7 are involved in melatonin signaling in Plasmodium falciparum. J. Pineal Res. 53: 147–153. DOI: 10.1111/J.1600-079X.2012.00981.X.
66. Bennink S, Pradel G (2019) The molecular machinery of translational control in malaria parasites. Mol. Microbiol. 112: 1658–1673. DOI: 10.1111/MMI.14388.
67. Lima WR, Moraes M, Alves E, Azevedo MF, Passos DO, Garcia CRS (2013) The PfNF-YB transcription factor is a downstream target of melatonin and cAMP signalling in the human malaria parasite Plasmodium falciparum. J Pineal Res 53: 145–153. DOI: 10.1111/j.1600-079X.2012.01021.x.
68. Maity SN, de Crombrugghe B (1998) Role of the CCAAT-binding protein CBF/NF-Y in transcription. Trends Biochem. Sci. 23: 174–178. DOI: 10.1016/S0968-0004(98)01201-8.
69. Kao CY, Tanimoto A, Arima N, Sasaguri Y, Padmanabhan R (1999) Transactivation of the human cdc2 promoter by adenovirus E1A. E1A induces the expression and assembly of a heteromeric complex consisting of the CCAAT box binding factor, CBF/NF-Y, and a 110-kDa DNA-binding protein. J. Biol. Chem. 274: 23043–23051. DOI: 10.1074/JBC.274.33.23043.
70. Hu Q, Bhattacharya C, Maity SN (2002) CCAAT binding factor (CBF) binding mediates cell cycle activation of topoisomerase IIalpha. Conventional CBF activation domains are not required. J. Biol. Chem. 277: 37191–37200. DOI: 10.1074/JBC.M205985200.
71. Lima WR, Holder AA, Garcia CRS (2013) Melatonin Signaling and Its Modulation of PfNF-YB Transcription Factor Expression in Plasmodium falciparum. Int. J. Mol. Sci. 14: 13704. DOI: 10.3390/IJMS140713704.
72. Lima WR, Tessarin-Almeida G, Rozanski A, Parreira KS, Moraes MS, Martins DC, Hashimoto RF, Galante PAF, Garcia CRS (2016) Signaling transcript profile of the asexual intraerythrocytic development cycle of Plasmodium falciparum induced by melatonin and cAMP. Genes Cancer 7: 323–339. DOI: 10.18632/genesandcancer.118.
73. Scarpelli PH, Tessarin‐Almeida G, Viçoso KL, Lima WR, Borges‐Pereira L, Meissner KA, Wrenger C, Rafaello A, Rizzuto R, Pozzan T, Garcia CRS (2019) Melatonin activates FIS1, DYN1, and DYN2 Plasmodium falciparum related‐genes for mitochondria fission: Mitoemerald‐GFP as a tool to visualize mitochondria structure. J. Pineal Res. 66: 14347–14352. DOI: 10.1111/JPI.12484.
74. Iwasawa R, Mahul-Mellier AL, Datler C, Pazarentzos E, Grimm S (2011) Fis1 and Bap31 bridge the mitochondria-ER interface to establish a platform for apoptosis induction. EMBO J. 30: 556–568. DOI: 10.1038/EMBOJ.2010.346.
75. Singh MK, Tessarin-Almeida G, Dias BKM, Pereira PS, Costa F, Przyborski JM, Garcia CRS (2021) A nuclear protein, PfMORC confers melatonin dependent synchrony of the human malaria parasite P. falciparum in the asexual stage. Sci. Rep. 11: 1–11. DOI: 10.1038/s41598-021-81235-2.
76. Moissiard G, Cokus SJ, Cary J, Feng S, Billi AC, Stroud H, Husmann D, Zhan Y, Lajoie BR, McCord RP, Hale CJ, Feng W, Michaels SD, Frand AR, Pellegrini M, Dekker J, Kim JK, Jacobsen SE (2012) MORC Family ATPases Required for Heterochromatin Condensation and Gene Silencing. Science 336: 1448–1451. DOI: 10.1126/science.1221472.
77. Weiser NE, Yang DX, Feng S, Kalinava N, Brown KC, Khanikar J, Freeberg MA, Snyder MJ, Csankovszki G, Chan RC, Gu SG, Montgomery TA, Jacobsen SE, Kim JK (2017) MORC-1 Integrates Nuclear RNAi and Transgenerational Chromatin Architecture to Promote Germline Immortality. Dev. Cell 41: 408-423.e7. DOI: 10.1016/j.devcel.2017.04.023.
78. Briquet S, Ourimi A, Pionneau C, Bernardes J, Carbone A, Chardonnet S, Vaquero C (2018) Identification of Plasmodium falciparum nuclear proteins by mass spectrometry and proposed protein annotation. PloS ONE 13: DOI: 10.1371/JOURNAL.PONE.0205596.
79. Pierce KL, Premont RT, Lefkowitz RJ (2002) Seven-transmembrane receptors. Nat. Rev. Mol. Cell Biol. 3: 639–650. DOI: 10.1038/NRM908.
80. Hall RA, Premont RT, Lefkowitz RJ (1999) Heptahelical receptor signaling: beyond the G protein paradigm. J. Cell Biol. 145: 927–932. DOI: 10.1083/JCB.145.5.927.
81. Madeira L, Galante PAF, Budu A, Azevedo MF, Malnic B, Garcia CRS (2008) Genome-wide detection of serpentine receptor-like proteins in malaria parasites. PLoS ONE 3: DOI: 10.1371/journal.pone.0001889.
82. Guha M, Maity P, Choubey V, Mitra K, Reiter RJ, Bandyopadhyay U (2007) Melatonin inhibits free radical-mediated mitochondrial-dependent hepatocyte apoptosis and liver damage induced during malarial infection. J. Pineal Res. 43: 372–381. DOI: 10.1111/j.1600-079X.2007.00488.x.
83. Ataide BJA, Kauffmann N, Mendes NSF, Torres MLM, Anjos LM. Passos ACF, Moraes SAS, Batista EJO, Herculano AM, Oliveira KRHM (2020) Melatonin prevents brain damage and neurocognitive impairment induced by plasmodium berghei anka infection in murine model of cerebral malaria. Front. Cell. Infect. Microbiol. 10: 541624 DOI: 10.3389/fcimb.2020.541624.
84. Kedarisetty CK, Samaga BL, Vidyasagar S, Venkataraman J (2020) Oral melatonin improves the detection of parasitemia in malaria. J. Infect. Dev. Ctries 14: 1327–1331. DOI: 10.3855/JIDC.12518.
85. Chagas disease - PAHO/WHO | Pan American Health Organization. https://www.paho.org/en/topics/chagas-disease. Accessed 17 Sep 2021.
86. Tyler KM, Engman DM (2001) The life cycle of Trypanosoma cruzi revisited. Int. J. Parasitol. 31: 472–481. DOI: 10.1016/s0020-7519(01)00153-9.
87. CDC - Chagas Disease. https://www.cdc.gov/parasites/chagas/index.html. Accessed 17 Sep 2021
88. Santos CD, Levy AM, Toldo MP, Azevedo AP, Prado JC (2007) Haematological and histopathological findings after ovariectomy in Trypanosoma cruzi infected mice. Vet. Parasitol. 143: 222–228. DOI: 10.1016/J.VETPAR.2006.08.038.
89. Santos CD, Caldeira JC, Toldo MPA, Prado JC (2005) Trypanosoma cruzi: Effects of repetitive stress during the development of experimental infection. Exp. Parasitol. 110: 96–101. DOI: 10.1016/J.EXPPARA.2005.03.009.
90. Santello FH, Frare EO, Santos CD, Caetano LC, Toldo MPA, Prado JC (2008) Suppressive action of melatonin on the TH-2 immune response in rats infected with Trypanosoma cruzi. J. Pineal Res. 45: 291–296. DOI: 10.1111/J.1600-079X.2008.00589.X.
91. Santello FH, Frare EO, dos Santos CD, Toldo MP, Kawasse LM, Zucoloto S, Prado JC (2007) Melatonin treatment reduces the severity of experimental Trypanosoma cruzi infection. J. Pineal Res. 42: 359–363. DOI: 10.1111/J.1600-079X.2007.00427.X.
92. Santello FH, Frare EO, Caetano LC, AlonsoToldo MP, Prado JC (2008) Melatonin enhances pro-inflammatory cytokine levels and protects against Chagas disease. J. Pineal Res. 45: 79–85. DOI: 10.1111/J.1600-079X.2008.00558.X.
93. Santello FH, del Vecchio Filipin M, Caetano LC, Brazão V, Caetano LN, Santos CD, AlonsoToldo MP, Prado JC (2009) Influence of melatonin therapy and orchiectomy on T cell subsets in male Wistar rats infected with Trypanosoma cruzi. J. Pineal Res. 47: 271–276. DOI: 10.1111/J.1600-079X.2009.00710.X.
94. Kuehn CC, Rodrigues Oliveira LG, Santos CD, Ferreira DS, Alonso Toldo MP, Albuquerque S, Prado JC (2009) Melatonin and dehydroepiandrosterone combination: does this treatment exert a synergistic effect during experimental Trypanosoma cruzi infection? J. Pineal Res. 47: 253–259. DOI: 10.1111/J.1600-079X.2009.00708.X.
95. Brazão V, Santello FH, Colato RP, Duarte A, Goulart A, Sampaio PA, Nardini V, Sorgi CA, Faccioli LH, Prado JC (2020) Melatonin down-regulates steroidal hormones, thymocyte apoptosis and inflammatory cytokines in middle-aged T. cruzi infected rats. Biochim. Biophys. Mol. Basis Dis 1866: 165914. DOI: 10.1016/J.BBADIS.2020.165914.
96. Brazão V, Colato RP, Santello FH, Vale GT, Gonzaga NA, Tirapelli CR, Prado JC (2018) Effects of melatonin on thymic and oxidative stress dysfunctions during Trypanosoma cruzi infection. J. Pineal Res. 65: e12510. DOI: 10.1111/JPI.12510.
97. Brazão V, Santello FH, Colato RP, Mazotti TT, Tazinafo LF, Toldo MPA, Vale GT, Tirapelli CR, Prado JC (2017) Melatonin: Antioxidant and modulatory properties in age-related changes during Trypanosoma cruzi infection. J. Pineal Res. 63: e12409. DOI: 10.1111/JPI.12409.
98. Brazão V, Filipin MDV, Santello FH, Caetano LC, Abrahão AMC, Toldo MPA, Prado JC (2011) Melatonin and zinc treatment: distinctive modulation of cytokine production in chronic experimental Trypanosoma cruzi infection. Cytokine 56: 627–632. DOI: 10.1016/J.CYTO.2011.08.037
99. Brazão V, Santello FH, Mdel FV, Azevedo AP, Toldo MP, Morais FR, Prado JC (2015) Immunoregulatory actions of melatonin and zinc during chronic Trypanosoma cruzi infection. J. Pineal Res. 58: 210–218. DOI: 10.1111/JPI.12207.
100. Oliveira LGR, Kuehn CC, dos Santos CD, Miranda MA, Costa CMB, Mendonça VJ, Prado JC (2013) Protective actions of melatonin against heart damage during chronic Chagas disease. Acta Trop. 128: 652–658. DOI: 10.1016/J.ACTATROPICA.2013.09.014.
101. Providello MV, Portapilla GB, Oliveira PAS, Silva CBP, Anchieta NF, Tirapelli CR, Albuquerque S (2020) Melatonin decreases circulating Trypanosoma cruzi load with no effect on tissue parasite replication. Can. J. Physiol. Pharmacol. 99: 795–802. DOI: 10.1139/CJPP-2020-0473.
102. Marsden PD (1986) Mucosal leishmaniasis (“espundia” Escomel, 1911). Trans. R. Soc. Trop. Med. Hyg. 80: 859–876. DOI: 10.1016/0035-9203(86)90243-9.
103. Ashford RW (2000) The leishmaniases as emerging and reemerging zoonoses. Int. J. Parasitol. 30: 1269–1281. DOI: 10.1016/S0020-7519(00)00136-3.
104. Alvar J, Vélez ID, Bern C, Herrero M, Desjeux P, Cano J, Jannin J, Boer M, Team the WHO Leishmaniasis Control (2012) Leishmaniasis worldwide and global estimates of its incidence. Plos ONE 7: e35671. DOI: 10.1371/JOURNAL.PONE.0035671.
105. Scott P, Novais FO (2016) Cutaneous leishmaniasis: immune responses in protection and pathogenesis. Nat. Rev. Immunol. 16: 581–592. DOI: 10.1038/nri.2016.72.
106. Gregory D, Oliver M (2005) Subversion of host cell signalling by the protozoan parasite Leishmania. Parasitology 130: S27–S35. DOI: 10.1017/S0031182005008139.
107. Laranjeira-Silva MF, Zampieri RA, Muxel SM, Floeter-Winter LM, Markus RP (2015) Melatonin attenuates Leishmania (L.) amazonensis infection by modulating arginine metabolism. J. Pineal Res. 59: 478–487. DOI: 10.1111/JPI.12279.
108. Elmahallawy EK, Jiménez-Aranda A, Martínez AS, Rodriguez-Granger J, Navarro-Alarcón M, Gutiérrez-Fernández J, Agil A (2014) Activity of melatonin against Leishmania infantum promastigotes by mitochondrial dependent pathway. Chem. Biol. Interact. 220: 84–93. DOI: 10.1016/J.CBI.2014.06.016.
109. Petronilli V, Penzo D, Scorrano L, Bernardi P, Di Lisa F (2001) The Mitochondrial Permeability Transition, Release of Cytochrome c and Cell Death: correlation with the duration of pore openings in situ. J. Biol. Chem. 276: 12030–12034. DOI: 10.1074/JBC.M010604200.
110. Baltaci AK, Bediz CS, Mogulkoc R, Kurtoglu E, Pekel A (2003) Effect of zinc and melatonin supplementation on cellular immunity in rats with toxoplasmosis. Biol. Trace Elem. Res. 96: 237–245. DOI: 10.1385/BTER:96:1-3:237.
111. Machado NI, dos Santos TAT, de Souza W, DaMatta RA, Seabra SH (2020) Treatment with melatonin induces a reduction of Toxoplasma gondii development in LLC-MK2 cells. Parasitol. Res. 119: 2703–2711. DOI: 10.1007/S00436-020-06766-5.
112. Majumdar T, Sharma S, Kumar M, Hussain MA, Chauhan N, Kalia I, Sahu AK, Rana VS, Bharti R, Haldar AK, Singh AP, Mazumder S (2019) Tryptophan-kynurenine pathway attenuates β-catenin-dependent pro-parasitic role of STING-TICAM2-IRF3-IDO1 signalosome in Toxoplasma gondii infection. Cell Death Dis. 10: (3): 161 DOI: 10.1038/S41419-019-1420-9.
113. Steinmann P, Keiser J, Bos R, et al (2006) Schistosomiasis and water resources development: systematic review, meta-analysis, and estimates of people at risk. Lancet Infect, Dis. 6: 411–425. DOI: 10.1016/S1473-3099(06)70521-7.
114. Abdallahi OM, Hanna S, de Reggi M, Gharib B (1999) Visualization of oxygen radical production in mouse liver in response to infection with Schistosoma mansoni. Liver 19: 495–500. DOI: 10.1111/J.1478-3231.1999.TB00082.X.
115. Caulfield JP, Lenzi HL, Elsas P, Dessein AJ (1985) Ultrastructure of the attack of eosinophils stimulated by blood mononuclear cell products on schistosomula of Schistosoma mansoni. Am. J. Pathol. 120: 380–390.
116. Kazura JW, Brito P de, Rabbege J, Aikawa M (1985) Role of granulocyte oxygen products in damage of Schistosoma mansoni eggs in vitro. J. Clin. Invest. 75: 1297–1307. DOI: 10.1172/JCI111830.
117. El-Sokkary GH, Omar HM, Hassanein AFMM, Cuzzocrea S, Reiter RJ (2002) Melatonin reduces oxidative damage and increases survival of mice infected with Schistosoma mansoni. Free Radic. Biol. Med. 32: 319–332. DOI: 10.1016/S0891-5849(01)00753-5.
118. Humans IWG on the E of CR to (1994) Infection with liver flukes (Opisthorchis viverrini, Opisthorchis felineus and Clonorchis sinensis). IARC Monogr. Eval. Carcinog. Risks Hum. 61: 121–175.
119. Sripa B, Kaewkes S, Sithithaworn P, Mairiang E, Laha T, Smout M, Pairojkul C, Bhudhisawasdi V, Tesana S, Thinkamrop B, Bethony JM, Loukas A, Brindley PJ (2007) Liver fluke induces cholangiocarcinoma. PLoS medicine 4: 1148–1155. DOI: 10.1371/JOURNAL.PMED.0040201.
120. Laothong U, Pinlaor P, Hiraku Y, Boonsiri P, Prakobwong S, Khoontawad J, Pinlaor S (2010) Protective effect of melatonin against Opisthorchis viverrini-induced oxidative and nitrosative DNA damage and liver injury in hamsters. J. Pineal Res. 49: 271–282. DOI: 10.1111/J.1600-079X.2010.00792.X.
121. Kim J, Cha YN, Surh YJ (2010) A protective role of nuclear factor-erythroid 2-related factor-2 (Nrf2) in inflammatory disorders. Mutat. Res. 690: 12–23. DOI: 10.1016/J.MRFMMM.2009.09.007.
122. Olivos-García A, Nequiz-Avendaño M, Tello E, Martínez RD, González-Canto A, López-Vancell R, García de León MC, Montfort I, Pérez-Tamayo R (2004) Inflammation, complement, ischemia and amoebic survival in acute experimental amoebic liver abscesses in hamsters. Exp. Mol. Pathol. 77: 66–71. DOI: 10.1016/J.YEXMP.2003.09.003.
123. França-Botelho AC, França JL, Oliveira FM, Franca EL, Honário-França AC, Caliari MV, Gomes MA (2011) Melatonin reduces the severity of experimental amoebiasis. Parasit. Vectors 4: 62. DOI: 10.1186/1756-3305-4-62.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.