Melatonin and the heart circadian clock of euglycemic and type 2 diabetic male rats: a transcriptional evaluation
Transcriptional effects of melatonin in the rat heart
Abstract
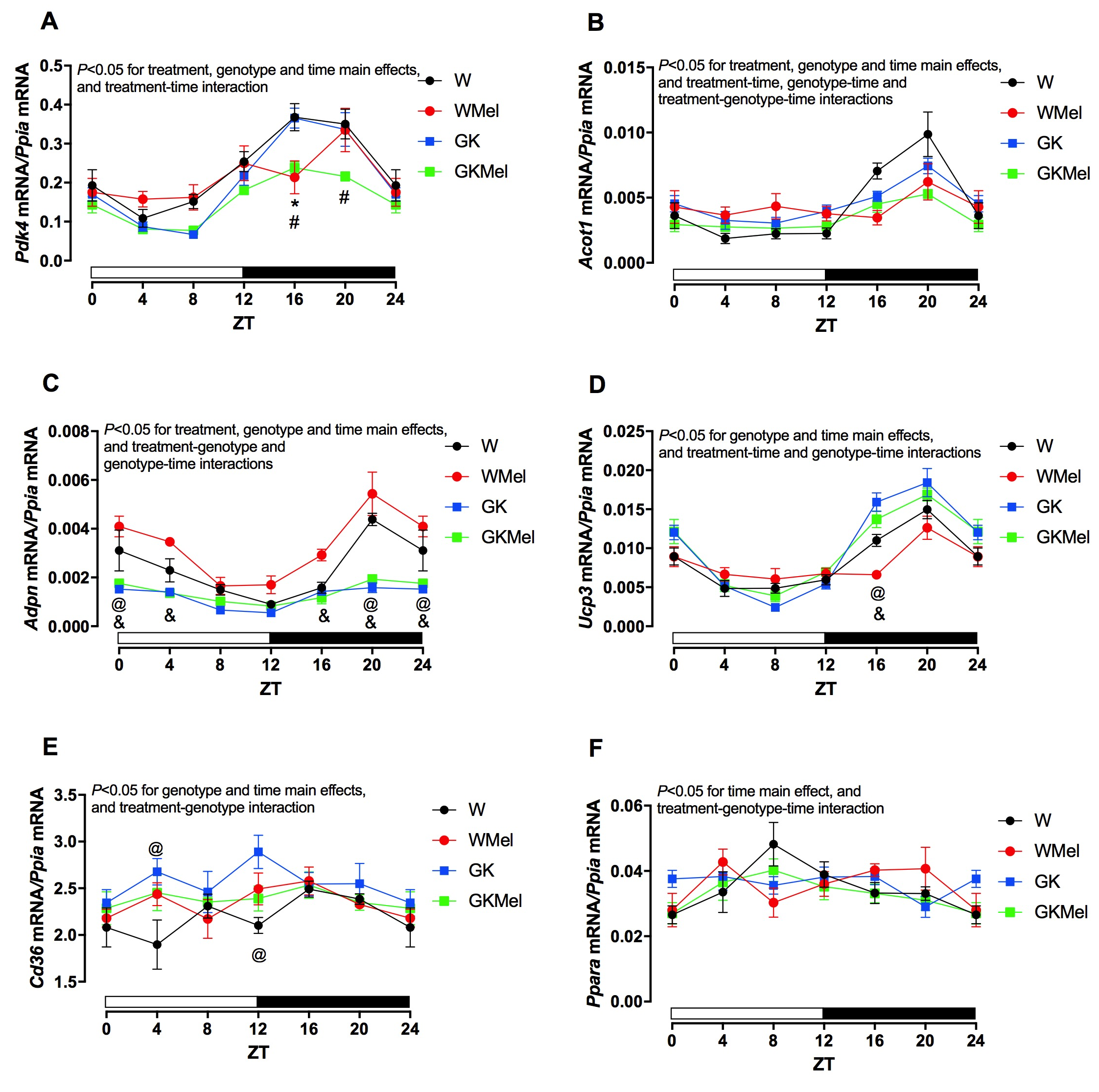
Diabetes increases risk of various comorbidities, including retinopathy, neuropathy, and cardiovascular disease, comprising both ischemic and non-ischemic cardiomyopathy. Cardiac dysfunction during diabetes is associated with perturbations at histologic, metabolic, biochemical and molecular levels. The circadian clock is misaligned in multiple organs during diabetes, including the heart. Such alterations in clock function have been postulated to play a causal role in cardiac dysfunction even though the mechanisms leading to circadian misalignment are currently unknown. Melatonin has been reported to alter heart circadian clock components and its circulating levels are decreased during diabetes. These observations led to the hypothesis that decreased melatonin levels during diabetes could be related to mismanagement of the heart clock. To evaluate this hypothesis, in the current study male Wistar and non-obese type 2 diabetic Goto-Kakizaki (GK) rats were given melatonin supplementation in their drinking water during the dark phase (for 12-wks), followed by assessment of clock component and the mRNA expression of the clock-controlled genes in the hearts of these animals. Melatonin supplementation significantly altered mRNA expression of targeted genes in both euglycemic and diabetic rat hearts. Collectively, under the condition of diabetes, the jeopardized pineal melatonin synthesis with misalignment of cardiac circadian clock components may likely mediate heart metabolic dysfunction, and/or even cause cardiovascular diseases.
References
2. Battiprolu PK, et al. (2010) Diabetic cardiomyopathy: Mechanisms and therapeutic targets. Drug Discov. Today Dis. Mech. 7 (2): e135-e143.
3. Echouffo-Tcheugui JB, et al. (2018) Diabetes mellitus and cardiogenic shock complicating acute myocardial infarction. Am. J. Med. 131 (7): 778-786 e771.
4. Bening C, et al. (2018) Impact of diabetes mellitus on the contractile properties of the left and right atrial myofilaments. Eur. J. Cardiothorac. Surg. 54 (5): 826-831.
5. Palomer X, et al. (2018) Emerging actors in diabetic cardiomyopathy: Heartbreaker biomarkers or therapeutic targets? Trends Pharmacol. Sci. 39 (5): 452-467.
6. Dubocovich ML, et al. (2003) Molecular pharmacology, regulation and function of mammalian melatonin receptors. Front. Biosci. 8: d1093-1108.
7. Witt-Enderby PA, et al. (2003) Melatonin receptors and their regulation: Biochemical and structural mechanisms. Life Sci. 72 (20): 2183-2198.
8. Peliciari-Garcia RA, et al. (2011) Expression of circadian clock and melatonin receptors within cultured rat cardiomyocytes. Chronobiol. Int. 28 (1): 21-30.
9. Kanikkannan N, et al. (2001) Evaluation of skin sensitization potential of melatonin and nimesulide by murine local lymph node assay. Eur. J. Pharm. Sci. 14 (3): 217-220.
10. Reiter RJ, et al. (2016) Melatonin as an antioxidant: Under promises but over delivers. J. Pineal Res. 61 (3): 253-278.
11. Baker J & Kimpinski K (2018) Role of melatonin in blood pressure regulation: An adjunct anti-hypertensive agent. Clin. Exp. Pharmacol. Physiol. 45 (8): 755-766.
12. Bertuglia S & Reiter RJ (2007) Melatonin reduces ventricular arrhythmias and preserves capillary perfusion during ischemia-reperfusion events in cardiomyopathic hamsters. J. Pineal Res. 42 (1): 55-63.
13. Genade S, et al. (2008) Melatonin receptor-mediated protection against myocardial ischaemia/reperfusion injury: Role of its anti-adrenergic actions. J. Pineal Res. 45 (4): 449-458.
14. Grossman E, et al. (2006) Melatonin reduces night blood pressure in patients with nocturnal hypertension. Am. J. Med. 119 (10): 898-902.
15. Lochner A, et al. (2018) Melatonin and cardioprotection against ischaemia/reperfusion injury: What's new? A review. J. Pineal Res. 65 (1):e 12490.
16. Sahna E, et al. (2008) Melatonin protects myocardium from ischemia-reperfusion injury in hypertensive rats: Role of myeloperoxidase activity. Clin. Exp. Hypertens. 30 (7): 673-681.
17. Sallinen P, et al. (2007) The effect of myocardial infarction on the synthesis, concentration and receptor expression of endogenous melatonin. J. Pineal Res. 42 (3): 254-260.
18. Simko F & Paulis L (2007) Melatonin as a potential antihypertensive treatment. J. Pineal Res. 42 (4): 319-322.
19. Yang Y, et al. (2014) A review of melatonin as a suitable antioxidant against myocardial ischemia-reperfusion injury and clinical heart diseases. J. Pineal Res. 5 7(4): 357-366.
20. Zhou H, et al. (2018) Protective role of melatonin in cardiac ischemia-reperfusion injury: From pathogenesis to targeted therapy. J. Pineal Res. 64 : e12471: 1-21.
21. Garcia RA, et al. (2008) Insulin modulates norepinephrine-mediated melatonin synthesis in cultured rat pineal gland. Life Sci. 82 (1-2):108-114.
22. Peliciari-Garcia RA, et al. (2010) Insulin temporal sensitivity and its signaling pathway in the rat pineal gland. Life Sci. 87 (5-6):169-174.
23. Amaral FG, et al. (2014) Melatonin synthesis impairment as a new deleterious outcome of diabetes-derived hyperglycemia. J. Pineal Res. 57 (1): 67-79.
24. Zhou H, et al. (2018) Melatonin therapy for diabetic cardiomyopathy: A mechanism involving syk-mitochondrial complex i-serca pathway. Cell Signal. 47: 88-100.
25. Bray MS, et al. (2008) Disruption of the circadian clock within the cardiomyocyte influences myocardial contractile function, metabolism, and gene expression. Am. J. Physiol. Heart Circ. Physiol. 294 (2): H1036-1047.
26. Young ME, et al. (2001) Intrinsic diurnal variations in cardiac metabolism and contractile function. Circulation Res. 89 (12): 1199-1208.
27. Durgan DJ & Young ME (2010) The cardiomyocyte circadian clock: Emerging roles in health and disease. Circulation Res. 106 (4): 647-658.
28. Durgan DJ, et al. (2006) The circadian clock within the cardiomyocyte is essential for responsiveness of the heart to fatty acids. J. Biol. Chem. 281 (34): 24254-24269.
29. Durgan DJ, et al. (2011) Evidence suggesting that the cardiomyocyte circadian clock modulates responsiveness of the heart to hypertrophic stimuli in mice. Chronobiol. Int. 28 (3): 187-203.
30. Young ME (2016) Temporal partitioning of cardiac metabolism by the cardiomyocyte circadian clock. Exp. Physiol. 101 (8): 1035-1039.
31. Chellappa SL, et al. (2019) Impact of circadian disruption on cardiovascular function and disease. Trends Endocrinol. Metab. S1043-2760 (19): 30131-30136. https://doi.org/10.1016/j.tem.2019.07.008
32. Young ME & Bray MS (2007) Potential role for peripheral circadian clock dyssynchrony in the pathogenesis of cardiovascular dysfunction. Sleep Med. 8 (6): 656-667.
33. Agez L, et al. (2007) Melatonin affects nuclear orphan receptors mRNA in the rat suprachiasmatic nuclei. Neuroscience. 144 (2): 522-530.
34. Dardente H, et al. (2003) Melatonin induces cry1 expression in the pars tuberalis of the rat. Brain Res. Mol. Brain Res. 114 (2): 101-106.
35. Owino S, et al. (2016) Melatonin signaling controls the daily rhythm in blood glucose levels independent of peripheral clocks. PloS one. 11 (1): e0148214.
36. Wagner GC, et al. (2007) Melatonin induces gene-specific effects on rhythmic mRNA expression in the pars tuberalis of the siberian hamster (phodopus sungorus). Eur. J. Neurosci. 25 (2): 485-490.
37. Zeman M & Herichova I (2013) Melatonin and clock genes expression in the cardiovascular system. Front. Biosci. (Schol. Ed). 5: 743-753.
38. Zeman M, et al. (2009) Effect of rhythmic melatonin administration on clock gene expression in the suprachiasmatic nucleus and the heart of hypertensive TGR(mRen2)27 rats. J. Hypertens. Suppl. 27 (6): S21-26.
39. Vriend J & Reiter RJ (2015) Melatonin feedback on clock genes: A theory involving the proteasome. J. Pineal Res. 58 (1): 1-11.
40. Kuwabara WMT, et al. (2017) Comparison of Goto-Kakizaki rats and high fat diet-induced obese rats: Are they reliable models to study type 2 diabetes mellitus? PloS one 12 (12): e0189622.
41. Mendes C, et al. (2013) Adaptations of the aging animal to exercise: Role of daily supplementation with melatonin. J. Pineal Res. 55 (3): 229-239.
42. Livak KJ & Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 25 (4): 402-408.
43. Dussault AA & Pouliot M (2006) Rapid and simple comparison of messenger RNA levels using real-time PCR. Biol. Proced. Online. 8: 1-10.
44. Peliciari-Garcia RA, et al. (2018) Repercussions of hypo and hyperthyroidism on the heart circadian clock. Chronobiol. Int. 35 (2): 147-159.
45. Peliciari-Garcia RA, et al. (2016) Interrelationship between 3,5,3 -triiodothyronine and the circadian clock in the rodent heart. Chronobiol. Int. 33 (10): 1444-1454.
46. Young ME, et al. (2001) Clock genes in the heart: Characterization and attenuation with hypertrophy. Circulation Res. 88 (11):1142-1150.
47. Nelson W, et al. (1979) Methods for cosinor-rhythmometry. Chronobiologia 6 (4): 305-323.
48. Cornelissen G (2014) Cosinor-based rhythmometry. Theor. Biol. Med. Model. 11: 16.
49. Cornelissen G, et al. (1980) Chronobiometry with pocket calculators and computer systems. Ric. Clin. Lab. 10 (2): 333-385.
50. Baker J & Kimpinski K (2018) Role of melatonin in blood pressure regulation: An adjunct anti-hypertensive agent. Clin. Exp. Pharmacol. Physiol. 45: 755-766.
51. Frese T, et al. (2009) Pineal melatonin synthesis is decreased in type 2 diabetic Goto-Kakizaki rats. Life Sci. 85 (13-14): 526-533.
52. Young ME, et al. (2002) Alterations of the circadian clock in the heart by streptozotocin-induced diabetes. J. Mol. Cell. Cardiol. 34 (2): 223-231.
53. Peliciari-Garcia RA, et al. (2016) Altered myocardial metabolic adaptation to increased fatty acid availability in cardiomyocyte-specific clock mutant mice. Biochim. Biophys. Acta. 1861 (10): 1579-1595.
54. Sarkozy M, et al. (2016) Transcriptomic alterations in the heart of non-obese type 2 diabetic Goto-Kakizaki rats. Cardiovasc. Diabetol. 15 (1): 110.
55. Bargi-Souza P, et al. (2015) Loss of basal and TRH-stimulated Tshb expression in dispersed pituitary cells. Endocrinology 156 (1): 242-254.
56. Mollard P, et al. (2012) A tridimensional view of pituitary development and function. Trends Endocrinol. Metab. 23 (6): 261-269.
57. Martino TA & Young ME (2015) Influence of the cardiomyocyte circadian clock on cardiac physiology and pathophysiology. J. Biol. Rhythms. 30 (3): 183-205.
58. Young ME (2017) Circadian control of cardiac metabolism: Physiologic roles and pathologic implications. Methodist Debakey Cardiovasc. J. 13 (1): 15-19.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.


